DNA methylation and diet are closely linked, with growing evidence suggesting that what you eat can impact how your genes function. This biochemical process acts like a dimmer switch for gene activity and is shaped by nutrients such as folate, B vitamins, and choline. These compounds do more than fuel your body—they help regulate gene expression, potentially affecting your health and even that of future generations. Learn how your daily diet plays a direct role in DNA methylation and why this connection matters for long-term well-being.
Key Takeaways
Diet directly influences DNA methylation, acting as a “dimmer switch” to regulate gene expression without altering the genetic code itself.
Key nutrients, including folate, B vitamins, choline, and methionine, serve as methyl donors, fueling the methylation process to support overall health and prevent conditions such as cancer, cardiovascular disease, and diabetes.
Personalized nutrition plans that incorporate genetic testing can optimize methylation, enabling tailored recommendations to align with individual genetic variations, such as MTHFR mutations.
Nutritional balance is crucial, as excess or deficiency in specific nutrients (e.g., folate, methionine, or polyphenols) can disrupt healthy methylation, leading to unintended health risks.
Whole, minimally processed foods rich in antioxidants and polyphenols, such as leafy greens, berries, fish, and turmeric, support protective methylation patterns, while processed foods may hinder them.
Lifestyle adjustments, such as regular exercise, stress management, and quality sleep, complement dietary strategies to maintain DNA health and balance methylation.
Table of Contents
Leveraging Diet to Modulate DNA Methylation in Clinical Practice
It’s incredible how much power lies on your plate—literally. In clinical practice, understanding the link between diet and DNA methylation offers a tangible way to guide your patients toward healthier outcomes. Let’s jump into why this epigenetic nutrition approach matters and how it plays out in real-life scenarios.
Why Practitioners Should Focus on Epigenetic Nutrition
Epigenetic nutrition is key to modern healthcare, with DNA methylation acting as a “dimmer switch” for gene activity. This process, driven by nutrients such as folate, B vitamins, and choline, helps regulate genetic expression without altering the DNA.
A diet rich in methylation-supportive foods, such as dark, leafy greens, can help mitigate the risks associated with genetic predispositions, including obesity, cancer, and metabolic disorders. Early-life nutrition is particularly crucial, as it influences lifelong health and reduces the risk of chronic diseases through epigenetic patterns established during the prenatal and early childhood stages.
Clinical Relevance of DNA Methylation
Diet can influence DNA methylation, affecting gene expression and potentially helping to prevent chronic illnesses such as diabetes and heart disease. This isn’t altering genetics but managing how genes are expressed through food choices. For example, in cases of fatigue caused by poor methylation due to an MTHFR gene variation, a diet rich in methyl donors, such as B12 and folate, significantly improves health without the need for heavy medication.
Aging alters methylation patterns, weakening immunity and accelerating cellular aging. Foods rich in polyphenols, such as green tea and berries, can support healthier methylation and help slow these changes. Genetic testing helps create personalized nutrition plans that target specific genes, such as FTO for obesity and APOE for cardiovascular risk. Through personalized dietary strategies, patients can gain control over their genetic expression, thereby improving their health outcomes.
Understanding DNA Methylation for Patient Care
Mechanisms of DNA Methylation
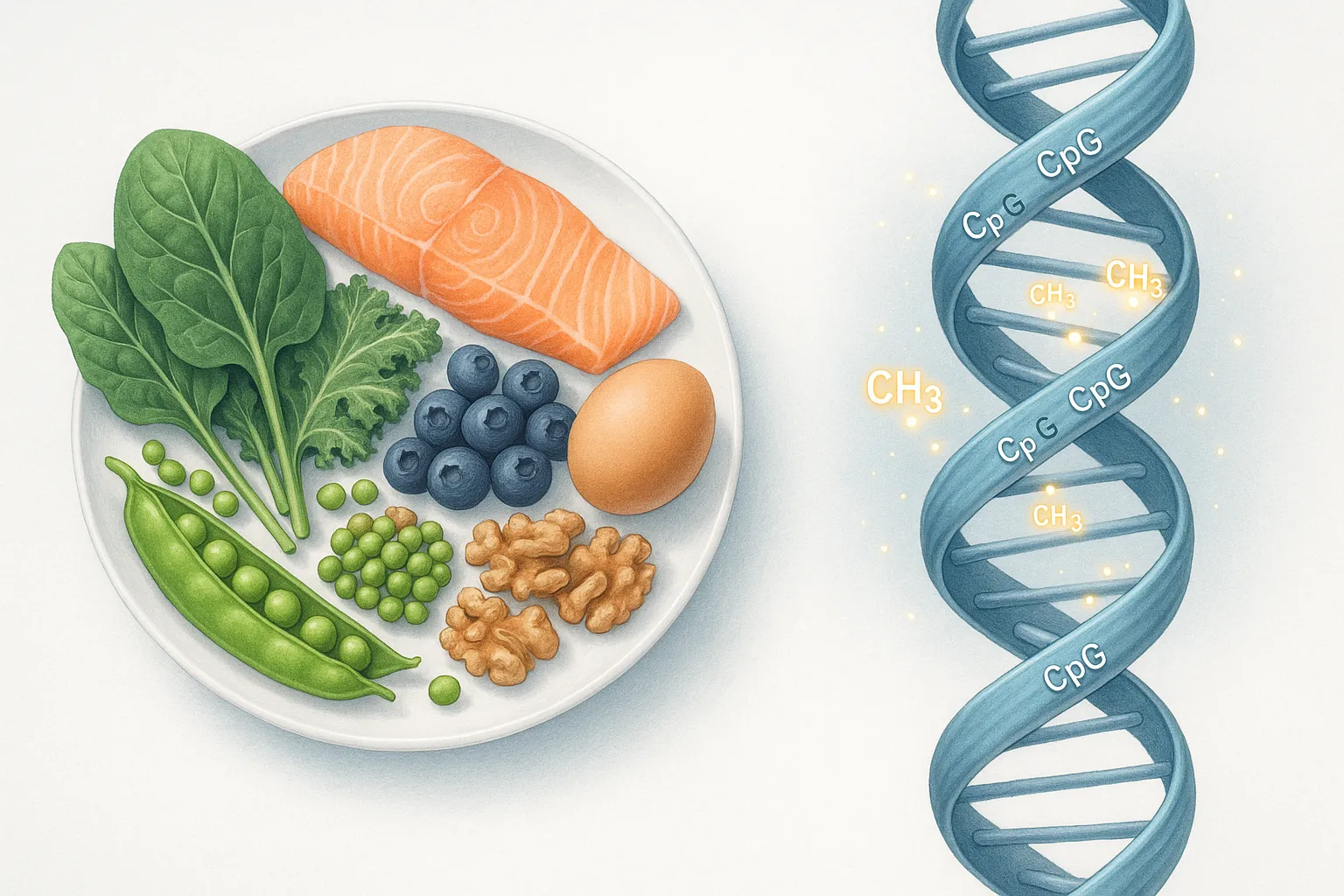
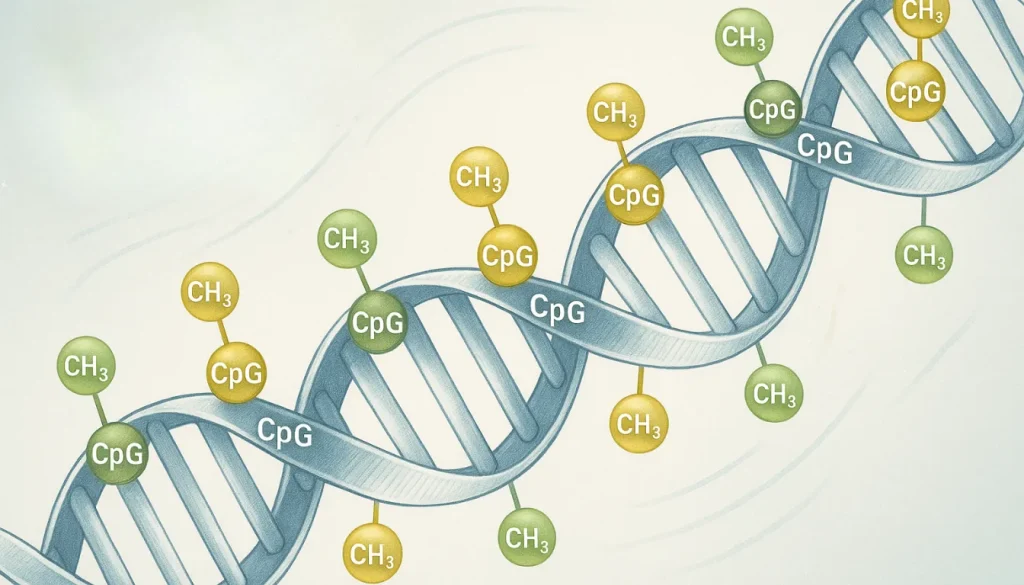
Think of DNA methylation like a dimmer switch for your genes. This process adds tiny chemical tags, known as methyl groups, to specific sites on your DNA, typically at CpG sites. When these tags latch on, they silence the gene, much like placing a “Do Not Disturb“ sign on a hotel door. This is an important way your body decides which genes to “turn on” or “turn off”, shaping everything from how your cells develop to how your body responds to a hearty serving of folate or B vitamins.
Diet plays a starring role here. Nutrients act as the key ingredients fueling this process, influencing everything from gene expression to cellular repair. By understanding exactly where these molecular “hats” land, you can guide your patients toward better health—one meal at a time.
Health and Condition Implications
Let’s face it: when it comes to health, DNA methylation can be both friend and foe. Proper methylation keeps your body’s complex machinery running smoothly, allowing it to repair cells and regulate systems. But when things go haywire—think chronic interruptions or nutrient deficiencies—you’re left with an increased risk of conditions like colorectal cancer, cardiovascular conditions, or diabetes.
Here’s a twist that blows many minds: your genes might load the gun, but your environment—diet, lifestyle, and stress—pulls the trigger. For instance, a high-sugar diet might disrupt methylation patterns, leaving you more vulnerable to inflammation-related diseases. By helping patients understand how their food affects their health, you’re offering them powerful tools to rewrite their life’s “genetic script”. And no, this isn’t sci-fi—it’s nutritional epigenomics at work.
Diet’s Role in Epigenetic Regulation
Picture this: your plate isn’t just holding dinner—it’s holding the power to influence your DNA. Foods like leafy greens, eggs, and fish are rich in methyl donors, which feed the methylation machine inside your body. It’s why those broccoli-and-spinach smoothies you’ve reluctantly tried to love might actually be genome superheroes.
One fascinating example? Studies reveal that omega-3 fatty acids can tweak DNA methylation patterns, particularly in pathways associated with inflammation and heart health. Imagine translating these findings into personalized advice for your patients—suddenly, recommending salmon for dinner isn’t just about protein, it’s about shaping their future health.
Diet’s influence on DNA isn’t just a theory—it’s a proven, powerful way to enhance patient outcomes without invasive treatments.
Mechanisms of Diet-Driven DNA Methylation
Your diet doesn’t just fuel your body—it’s like a backstage crew, quietly pulling strings that influence how your genes behave. If you’ve ever wondered how the foods you eat can flip genetic switches, you’re not alone. Understanding these mechanisms helps you harness this power by tweaking your diet to promote health and prevent certain conditions.
One-Carbon Metabolism in Clinical Context
One-carbon metabolism, fueled by nutrients like folate, vitamin B12, and methionine, provides methyl groups that help regulate gene activity through DNA methylation. These methyl groups act as tags that control gene expression.
Without these nutrients, gene regulation may fail, raising risks for diseases like cancer, heart issues, or neurological disorders. Nutritional epigenomics examines how diet influences gene expression, highlighting the benefits of consuming foods like leafy greens, eggs, and fish in optimizing DNA regulation.
Research Evidence for Practitioners
Observational studies show clear links between diet and DNA methylation changes in conditions such as obesity, cancer, and even among healthy people. For example, a high intake of folate has been shown to prevent global DNA hypomethylation, which, in simpler terms, means maintaining a stable “on and off” switch for your genes. But it’s not just deficiencies you need to worry about—too much methionine, found in abundance in protein sources like meat, can lead to hypermethylation, potentially silencing essential genes.
The overlooked complexity here is striking. Nutrient imbalances, whether too little or too much, create a domino effect on methylation patterns. If you’re designing personalized nutrition for nutrigenomics, consider these nuances—the line between effective interventions and unintended consequences is surprisingly thin.
Pitfalls in Dietary Interventions
Here’s a common pitfall: assuming every nutrient works the same way. Spoiler alert—it doesn’t. Some nutrients, like polyphenols found in berries or green tea, can inhibit DNA methylation. This disruption can be protective in certain situations, such as targeting cancer cells, but it can be harmful when it indiscriminately silences genes in healthy tissues. Balance is everything here.
Another trap? Overlooking genetic variations. If someone has an MTHFR mutation, for instance, they might process folate differently. This means a standard “folic acid fortification” won’t suffice—they’ll need activated forms, such as methylfolate, to reap the benefits. Ignoring these genetic quirks can render dietary interventions not only ineffective but also potentially harmful.
Nutrients Impacting DNA Methylation: A Practitioner’s Guide
When it comes to diet and gene expression, the foods we eat don’t just fuel our bodies—they send instructions to our genes, flipping switches that can influence everything from metabolism to condition prevention. For practitioners like you, understanding how nutrients impact DNA methylation can feel like revealing a toolkit for tailored patient care. Let’s unpack the key players in this biochemical dance and how you can harness their potential.
Methylation-Promoting Nutrients
Think of these nutrients as the “builders” of the DNA methylation process—they stabilize and optimize gene expression by supplying the tools needed for proper methylation.
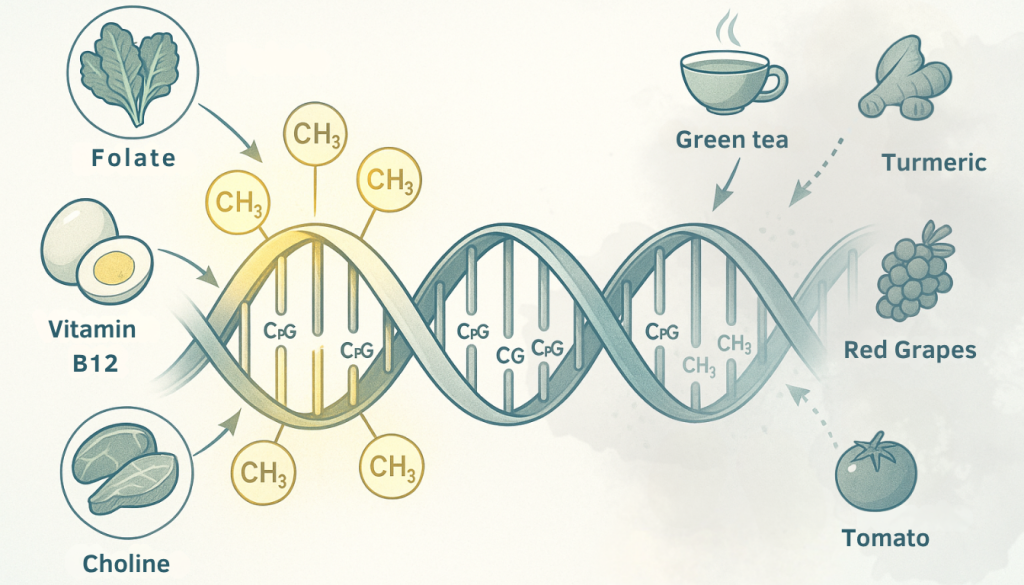
Folate: This vitamin is the MVP of the one-carbon pathway. Found in leafy greens (such as spinach and kale) and legumes, it acts as a scaffold supporting methylation. But here’s a twist—while folate is essential, high doses—especially from supplements—might increase cancer risks in susceptible individuals. It’s nature’s version of “too much of a good thing.”
Vitamin B12: This nutrient acts like a supervisor, ensuring your methylation machinery runs smoothly. You’ll find it in meats, fish, and eggs. Without B12, the methionine cycle—a critical route in the process—can stumble, leaving your body’s repair system in a jam.
Methionine: Known as a heavy hitter in poultry, dairy, and certain seeds, methionine transforms into S-adenosylmethionine (SAM), a powerhouse donor of methyl groups. Caution, though: excessive methionine has been tied to potential neurological challenges, so balance is key.
Choline, Betaine, Vitamins B2 and B6: Consider these the supporting actors that ensure enzymatic reactions proceed. Choline (found in eggs and liver), betaine (found in beets and spinach), and B vitamins work together to maintain proper methylation flow, a critical step in preventing dietary influences on DNA disruptions.
Methylation-Inhibiting Nutrients
On the flip side, some nutrients act like story editors, tweaking or even disrupting sections of DNA methylation. Their effects depend on context and quantity, so they’re more of a double-edged sword.
Tea Polyphenols (EGCG): Straight from your green tea mug, these compounds are known to decrease global methylation levels when consumed in high doses. For some genes, this can mean reduced cancer risk, but for others, it might cause problems if overdone.
Resveratrol, Curcumin, Lycopene: Think of these as the natural “erasers” for certain methylation marks. Found in red grapes (resveratrol), turmeric (curcumin), and tomatoes (lycopene), they promote gene expression by lowering excessive methylation on silenced genes. However, moderation matters—adding turmeric to your soup is beneficial, yet excessive supplement use can have adverse effects.
Vitamin C: A classic immune-boosting favorite, this fruity friend also plays a role in demethylating DNA, particularly in stem cells. It serves as a reminder of how nutrients can influence genetic changes with significant health implications.
Nutrient Reference Table
Nutrient | Effect on Methylation | Food Sources | Notes |
|---|---|---|---|
Methylation Food Sources | Increases | Leafy greens, legumes | Essential, but avoid excess in supplements |
Vitamin B12 | Increases | Meat, fish, eggs | Important for the methionine cycle |
Methionine | Increases | Poultry, dairy, and seeds | Excess tied to neurological risk |
Choline | Increases | Eggs, liver, cauliflower | Precursor to betaine |
Tea Polyphenols | Inhibits | Green tea | High doses lower global methylation |
Curcumin | Inhibits | Turmeric | Enhances cancer assistance response |
Lycopene | Inhibits | Tomatoes, carrots | Linked to hypomethylation |
Optimizing Nutrient Balance in Practice
Here’s the golden rule for practitioners: Balanced cells are like well-tuned orchestras—functional but sensitive to disruption. Your job is to maintain harmony in methylation by personalizing nutrition plans.
Key Insight: Healthy methylation often thrives on a Goldilocks principle. Normal consumption of inhibitors (like polyphenols from a few cups of green tea or a sprinkle of turmeric) is unlikely to tip the scales negatively. However, when supplements or excessive doses are used without proper testing, it can lead to nutritional chaos.
Mistake to Avoid: Overprescribing supplements without understanding a patient’s genetic blueprint is a risky practice. Tools like genetic testing (yes, even sophisticated ones like “Elite Gene Labs”) can help you avoid creating imbalances that harm the epigenetic changes diet is supposed to support.
Dietary Patterns and Epigenetic Outcomes in Patient Populations
Let’s explore how specific dietary patterns influence epigenetic outcomes in various patient groups.
Paleo Diet as a Solution
The Paleo diet, often called the “caveman diet”, focuses on whole foods like lean meats, fish, veggies, fruits, nuts, and seeds. This diet is less about reenacting history and more about cutting modern-day junk—no ultra-processed foods stuffed with fillers that mess with your body’s natural rhythms. From an epigenetic standpoint, the Paleo diet supports stable DNA methylation by providing key nutrients like choline and B vitamins, which act as essential “methyl donors”.
Patients with chronic diseases like diabetes or obesity often see positive shifts when switching to this grain-free, sugar-free eating plan. Why? Because epigenetic changes from poor diets rich in processed carbs tend to fuel inflammation. Paleo flips the script by nourishing your genes with whole, unprocessed goodness. Just remember, moderation matters—overdoing red meat, for instance, might counteract the benefits depending on individual genetic predispositions.
Mediterranean Diet as a Clinical Tool
The Mediterranean diet is the red-carpet darling of dietary interventions, and for a good reason. Packed with fresh veggies, fruits, whole grains, nuts, fish, and healthy fats like olive oil, it’s essentially brain food that’s also heart-friendly. From an epigenetic perspective, this diet promotes a balanced methylation profile that supports longevity and reduces risk factors for diseases.
Studies have shown that Mediterranean diets don’t just help you feel good—they may slow down aging at the epigenetic level. A low-sugar version of this diet has been linked to delayed epigenetic aging, making it a go-to recommendation for patients seeking preventive health measures. To help patients make the change, suggest simple swaps, such as trading butter for olive oil or snacking on almonds instead of chips. These small, doable changes let your DNA reap big rewards. After all, dietary influence on DNA isn’t magic—it’s mindful eating.
Vegan vs. Omnivore Diets: Clinical Considerations
If you’ve ever wondered how a vegan diet stacks up against a traditional omnivore approach when it comes to epigenetics, the answer is—it depends. Research—including twin studies—shows vegan diets can favorably influence epigenetic clocks, leaving vegans with potentially “younger” gene expression. The diet’s plant-heavy focus provides phytonutrients and antioxidants, which are essential for combating oxidative stress, a process that can otherwise disrupt DNA methylation patterns.
Vegan diets may lack vitamin B12, a key player in methylation processes. If you have a vegan patient, emphasize the importance of supplementation to avoid methyl-group shortages that could derail the health benefits. On the other hand, omnivorous diets are naturally richer in B12. Still, they may require careful attention to reduce the consumption of processed meats or unhealthy fats that can counteract the positive epigenetic outcomes. The key here is balance—whether you’re a vegan or an omnivore, it’s all about what you put on your plate.
Risks of Processed Food Diets
Processed foods can negatively impact your DNA by disrupting epigenetic regulation, which may increase the risk of diseases like cancer, heart issues, and cognitive decline. These foods, which are often packed with additives, trans fats, and excess sugar, can lead to harmful changes in DNA methylation, potentially activating harmful genes and silencing protective ones.
To protect your DNA, focus on whole, minimally processed meals—like fresh vegetable stir-fries with turmeric—instead of processed options. Small, healthy diet changes can make a big difference.
Clinical Implications of Diet-Induced Methylation Changes
DNA methylation isn’t just some obscure biology term—it’s like a molecular switchboard dictating how your genes behave. And the food you eat? It’s one of the control levers. Decoding this connection can help you manage patient health more effectively, especially if you’re in the business of tailoring nutrition plans. Let’s break down how these dietary epigenetic tweaks impact major health areas.
Condition Risk Mitigation
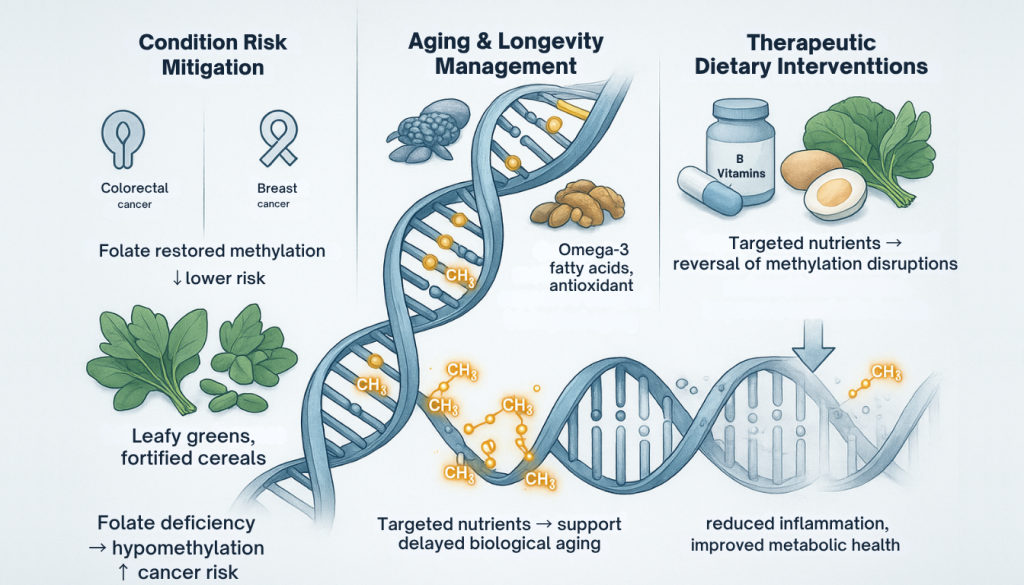
Think of DNA methylation as a traffic controller for your genes. When it’s balanced, the traffic flows smoothly, preventing pile-ups like those associated with cancer or heart conditions. But when things go haywire—say, folate deficiency causes hypomethylation—your patients might find themselves at a higher risk of colorectal or breast cancers. It’s like forgetting to check your tire pressure before a road trip—a small oversight with major, sometimes preventable, consequences.
Heart condition and diabetes, two heavy-hitters in the chronic condition world, are also tied to methylation irregularities. Tweaking methylation through wise dietary choices has the potential to cut condition risk by up to 30%, according to some studies. Pretty impressive, right? Here’s the play: guide your patients toward folate-rich foods, such as leafy greens or fortified cereals. It’s a little like upgrading their car’s oil filter—simple but essential for long-term performance.
Aging and Longevity Management
Dietary patterns rich in vitamin D, omega-3 fatty acids, and antioxidants have been shown to influence these aging markers effectively. It’s like treating your DNA to a spa day, helping to slow biological aging while boosting overall vitality. Yet so many patients focus on counting calories instead of the quality of their nutrition, missing out on this fountain-of-youth effect. Why not educate your practice about foods that support methylation balance—such as fatty fish, nuts, and berries—to buy more quality years over quantity years?
Therapeutic Dietary Interventions
Some diet-induced methylation changes aren’t irreversible—yes, you can reverse course, at least partially. Think of it as editing a poorly written draft for smoother, healthier outcomes. By introducing a targeted dietary strategy, patients under your care may experience measurable improvements in areas such as inflammation, metabolic disorders, or even brain health.
This approach isn’t without its fuzzy areas. While we know that dietary shifts are effective, more rigorously designed studies are still needed to link specific diet-to-methylation pathways definitively. But that doesn’t mean you can’t get started. Testing the waters with evidence-backed staples, such as boosting folate, choline, or vitamin B12 intake offers a chance to reset those molecular switches toward a healthier narrative for your patients.
Nutrigenomics in Functional Medicine Practice
Personalized Nutrition Protocols
Imagine being able to design a patient’s diet as perfectly as a tailored suit—this is what nutrigenomics allows you to do. By analyzing genetic profiles, particularly those related to methylation, such as MTHFR and COMT, you can tailor a person’s diet to their unique genetic needs. It’s like discovering your DNA’s favorite “playlist” of nutrients. For example, someone with an MTHFR gene variation might need more folate-rich foods (think spinach, avocados, and beans) to support proper methylation. When you match these needs, you’re not just managing signs—you’re actively reducing risks for conditions such as cardiovascular disease and diabetes. This isn’t guesswork anymore; it’s precision care at its finest.
Integrating Genetic Testing with Elite Gene Labs
Think of genetic testing as a flashlight that reveals what your patient’s DNA is up to behind the scenes. Services like Elite Gene Labs make it easy to highlight methylation quirks that might otherwise remain hidden. Let’s say a test comes back showing an MTHFR mutation—this tells you to amp up methylation-friendly folate in their diet. Broccoli? Yes, please. Folate supplements? Maybe, if needed. You’re essentially giving each patient a treasure map to optimal health, one nutrient at a time. And the best part? These tailored nutrition strategies help unlock better energy, sharper focus, and even improved longevity for your patients.
Avoiding Generic Nutrition Plans
Generic meal plans are like one-size-fits-all t-shirts—they might work, but they rarely fit well. If you’re not accounting for someone’s genetic map, you could miss the mark completely. A trendy low-carb diet might backfire if their genes crave more complex carbs for energy regulation. Or perhaps that high-protein plan risks overloading their kidneys. Ignoring individual DNA quirks could disrupt the delicate balance of dietary influence on DNA, leading to subpar (or worse, harmful) results. When you skip the cookie-cutter approach and prioritize personalized plans, you’re not just helping patients feel better—you’re helping them thrive at their very core.
Practical Strategies for Practitioners to Optimize Patient Methylation
Helping patients balance DNA methylation might sound like science fiction, but it’s surprisingly tangible. Think of it as teaching their genes to behave appropriately, like a well-directed play where every actor knows their role. Here’s how you can support this intricate process with nutrition, lifestyle tweaks, and cutting-edge tools.
Recommended Dietary Interventions
Start with the essentials: load your patient’s plate with foods rich in methylation supporters. Folate is the star here—imagine those deep greens like spinach and kale, lentils, or even fortified cereals acting as the stage crew, setting everything up behind the scenes. Add vitamin B12 to your diet through foods like meat, fish, or eggs. And let’s not forget methionine, which is found in poultry and dairy, quietly keeping things running smoothly in the background.
Encourage patients to experiment with colorful plates—plump berries, zingy turmeric, or even garlic add both variety and vital nutrients to their diet. These simple additions not only make meals vibrant but also bolster their epigenetic health. Want a pro tip? Suggest they sip on green tea, but don’t overdo it—balance is key to avoid tipping methylation into overdrive.
Nutrients to Monitor
Even the best things in life can turn counterproductive if consumed in excess. Take green tea polyphenols and resveratrol, for instance. While these compounds have glamorous reputations in the wellness world, going overboard could hinder methylation. Please suggest moderation, especially if their genetic data shows sensitivity.
Processed foods are the real villains in the methylation story. These ultra-processed items aren’t just empty calories; they can disrupt epigenetic balance entirely. Think of it like static cutting into a beautiful symphony. Guide patients toward whole, minimally processed choices—it’s like wiping the slate clean for their DNA to play its proper tune.
Complementary Lifestyle Interventions
Diet is a massive piece of the puzzle, but it’s not everything. Encourage patients to embrace a holistic approach. Regular movement—whether it’s yoga, a brisk walk, or their favorite sport—helps optimize methylation. Pair that with quality sleep, and their genes will practically thank them.
Don’t forget stress management. Chronic stress is like letting a neurotic stage manager take over—it throws the whole production off. Offer mindfulness techniques, deep breathing exercises, or even journaling as ways to keep stress in check. These small steps can make a significant impact on their overall DNA harmony.
Implementing Genetic Testing in Practice
Now this is where it gets exciting! By integrating genetic testing—think a service like Elite Gene Labs—you can seriously up your game. Imagine handing patients a personalized report and saying, “Here’s what your diet should look like to optimize your methylation.” It’s like giving them a custom cheat sheet for their health.
By uncovering their methylation profile, you can make hyper-targeted nutrition plans that align with their unique epigenomic needs. This doesn’t just mean better indicator management; it unlocks the full potential of nutritional epigenomics, from reducing the risks of chronic illness to slowing the effects of aging.
Conclusion: Advancing Patient Outcomes Through Epigenetic Nutrition
Your diet holds incredible power to shape your health at the genetic level. By understanding DNA methylation and diet, you can make smarter food choices that support not just your well-being but potentially that of future generations.
Personalized nutrition, guided by genetic insights, provides a practical approach to addressing health challenges and reducing condition risks. When you align your dietary habits with your unique genetic profile, you’re taking a proactive step toward better health outcomes.
This approach isn’t just transformative—it’s empowering. Small, intentional changes to your diet can have a ripple effect, enhancing your health in ways that go far beyond the plate.
Frequently Asked Questions
What is DNA methylation, and why is it important?
DNA methylation is a natural process where methyl groups are added to DNA, acting like a dimmer switch to control gene activity. It plays a crucial role in regulating genes, maintaining cellular health, and preventing disease. Proper methylation supports cell repair and function, while imbalances can increase the risk of diseases such as cancer and diabetes.
Which nutrients are essential for DNA methylation?
Nutrients such as folate, vitamin B12, choline, methionine, and vitamin B6 are vital for DNA methylation. These nutrients, known as methyl donors, help regulate gene expression and support overall health.
How does diet influence DNA methylation?
Diet provides nutrients that affect DNA methylation processes. Consuming a balanced diet rich in methyl donors, such as leafy greens, eggs, and fish, can promote proper methylation, while processed foods and nutrient deficiencies may disrupt this process.
Can DNA methylation influence health conditions such as obesity and heart disease?
Yes, improper DNA methylation can influence the expression of genes linked to obesity and cardiovascular diseases. Personalized nutrition plans can help manage such conditions by targeting methylation pathways.
What foods enhance DNA methylation?
Foods rich in methylation-supporting nutrients include leafy greens (folate), eggs (choline), fish and poultry (vitamin B12), and legumes. These foods help maintain a balanced methylation process.
Can methylation patterns be inherited?
Yes, DNA methylation patterns can be passed to future generations, influencing predispositions to specific health conditions. Early-life nutrition plays a significant role in shaping these patterns.
What diets are best for optimizing DNA methylation?
Diets like the Mediterranean diet, which emphasize whole foods and a balanced intake of nutrients, support healthy methylation. The Paleo diet has also shown positive effects, but processed food diets should be avoided.
How can genetic testing help with personalized nutrition?
Genetic testing identifies individual variations in methylation-related genes, enabling healthcare practitioners to tailor dietary recommendations to optimize health outcomes and mitigate disease risks.
Are vegan diets good for DNA methylation?
Vegan diets can have a positive impact on DNA methylation, but they may lack crucial nutrients, such as vitamin B12, which is essential for proper methylation. Supplementing as needed ensures a balanced dietary approach.
How can poor methylation be corrected?
You can improve methylation by eating whole, unprocessed foods rich in folate, B vitamins, and choline. Managing stress, regular exercise, and avoiding nutrient deficiencies also support healthy methylation.

